Radiology Tutor
Tumour volume doubling time
The formula used for the above calculator is (1):
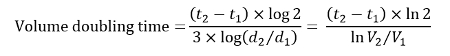
Where t1 is the initial study time, t2 the follow up study time with (t2-t1) the interval, d1 and V1 are the diameter and volume at the time of the first study, and d2 and V2 are the diameter and volume at the time of the second study.
This assumes a spherical tumour with exponential growth (one cell divides to two, two to four, and so on).
The accepted guidelines for the follow up of solitary pulmonary nodules ≤8 mm detected incidentally on CT are the Fleischner guidelines(2). These rely on a single measurement in the axial plane. We know that the measurement of pulmonary nodules <20 mm is associated with interobserver variability(3) and that semi-automated volume measurements may reduce interobserver variability(4,5), but segmentation problems still hamper volume analysis(6-8). Tumour doubling time has been used to differentiate benign from malignant nodules(9), but the studies are limited by low numbers and it is clear that there is a wide variation in doubling times of malignant tumours(9,10). For these reasons, volume doubling time is not a useful clinical tool in most cases. The Fleischner Society guidelines can be found here.
References
- Schwartz, M. A biomathematical approach to clinical tumor growth. Cancer 14, 1272–1294 (1961).
- MacMahon, H. et al. Guidelines for Management of Small Pulmonary Nodules Detected on CT Scans: A Statement from the Fleischner Society 1. Radiology 237, 395–400 (2005).
- Revel, M.-P. et al. Are Two-dimensional CT Measurements of Small Noncalcified Pulmonary Nodules Reliable?1. Radiology 231, 453–458 (2004).
- Revel, M.-P. et al. Pulmonary Nodules: Preliminary Experience with Three-dimensional Evaluation1. Radiology 231, 459–466 (2004).
- Goodman, L. R., Gulsun, M., Washington, L., Nagy, P. G. & Piacsek, K. L. Inherent variability of CT lung nodule measurements in vivo using semiautomated volumetric measurements. Ajr Am. J. Roentgenol. 186, 989–994 (2006).
- Petrou, M., Quint, L. E., Nan, B. & Baker, L. H. Pulmonary nodule volumetric measurement variability as a function of CT slice thickness and nodule morphology. Ajr Am. J. Roentgenol. 188, 306–312 (2007).
- Gietema, H. A. et al. Pulmonary nodules detected at lung cancer screening: interobserver variability of semiautomated volume measurements. Radiology 241, 251–257 (2006).
- Gietema, H. A., Schaefer-Prokop, C. M., Mali, W. P. T. M., Groenewegen, G. & Prokop, M. Pulmonary nodules: Interscan variability of semiautomated volume measurements with multisection CT-- influence of inspiration level, nodule size, and segmentation performance. Radiology 245, 888–894 (2007).
- Revel, M.-P. et al. Software volumetric evaluation of doubling times for differentiating benign versus malignant pulmonary nodules. Ajr Am. J. Roentgenol. 187, 135–142 (2006).
- Quint, L. E., Cheng, J., Schipper, M., Chang, A. C. & Kalemkerian, G. Lung lesion doubling times: values and variability based on method of volume determination. Clin. Radiol. 63, 41–48 (2008).
- Wilson, D. O. et al. Doubling Times and CT Screen-Detected Lung Cancers in the Pittsburgh Lung Screening Study. Am. J. Respir. Crit. Care Med. 185, 85–89 (2012).